Terminally Ill Patients in Canada Face Same Hospice Enrollment Problems as U.S.
One of the most pressing challenges in hospice is the delaying of hospice enrollment until the final days of a patient’s life. In the U.S., physicians prefer to continue aggressive treatments long after a terminal diagnosis, which may extend a patient’s life but diminished their quality of life. Recent research from Canada has shown that this is not a problem unique to the U.S. In fact, nearly 70 percent of seriously ill patients in Canada received invasive end-of-life treatments they did not need or want.
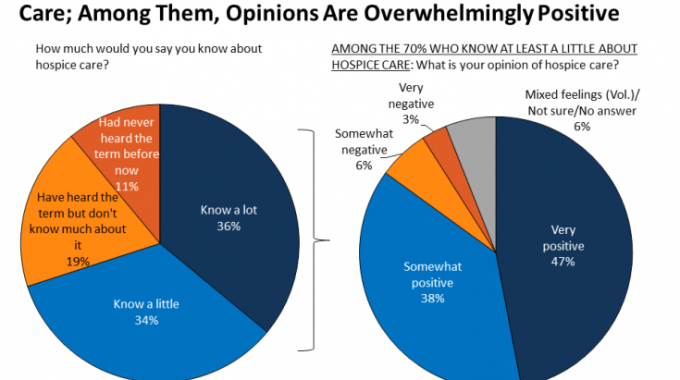
A recent Kaiser Family Foundation survey found that most people have a favorable view of hospice. Despite the trend, hospice enrollment continues to be delayed in most patients until their final moments when hospice’s effectiveness is limited. Hospice helps patients through their final life transition and aims to make their last days comfortable and as enjoyable as possible. Earlier enrollment in hospice is directly linked to higher satisfaction with care.
Canada’s hospice enrollment problem
For the past decade, a Canadian group called CARENET has sought to bring light to the issue of late hospice enrollment. What they found through their research is startling. While patients often discussed their wishes for end-of-life care with their families, only 17.0% of patients and 18.2% of family members had discussed their preferences with a specialist physician, and only 30.3% of patients and 22.6% of family members had discussed their choices with a family physician. The failure to engage with physicians in end-of-life discussions was found to correlate with late hospice enrollment directly.
One study found that most patients and their families prefer comfort in care, but in most cases life-sustaining treatments continued and a majority of patients died in an acute care setting. Another study found more troubling problems in hospice enrollment when it found that fewer than 7% of terminally ill patients died in a hospice in some parts of Canada. Over 87% of terminally ill patients died in an acute care setting in Quebec, the study found. These results speak to a significant problem in how the Canadian medical system as a whole treats terminally ill patients.
Communication is key
Part of the problem may stem from a breakdown in communication between patients and their physicians. As discussed above, only a small percentage of patients and families engage physicians in end-of-life discussions. Shockingly, many terminally ill patients have no idea they are dying. In a recent article penned for the online journal Practical Pain Management, Dr. Jessica Zitter, a palliative care physician and author, explains, “In the absence of shared knowledge of this critical information with the patient, there is a tendency for the patient to get shuttled onto what I have come to call the ‘end-of-life conveyor belt.’ When a fatal condition is not acknowledged, patients may be submitted to end-of-life medical care where they are given increasing levels of life-prolonging technology and medications. Ample data support an evident reluctance, even opposition, to this kind of harsh treatment.”
Physicians want to do what is best for their patients, but many feel sending those under their care to hospice is a sign that they have given up, so they persevere with more treatments. The last thing a physician wants is for a patient to feel medically abandoned. Without a candid discussion about a patient’s end-of-life wishes, a physician will likely delay hospice in favor of life-extending treatments, even when the patient does not want those treatments. The solutions to improving hospice enrollments rest with the strength of communication between hospice patients and their physicians (and families, too).
Hospice improves satisfaction in care
It is a well-studied and well-documented fact that hospice improves satisfaction in care among patients. The ultimate goal is to offer patients a good death. A study conducted on this topic explored 36 peer-reviewed research papers, each of which made some attempt to define what we consider to be “a good death.” Some of the core themes identified were:
- An experience free from pain.
- A preference for a specific way to pass on.
- Religious, spiritual, and emotional well-being.
- Achievements in life and continuing quality of life.
- Preferences for – and limitations of – treatments permitted.
- Passing on with dignity, in the company of friends and loved ones.
Patients overwhelmingly placed a particular form of dying atop the list of important considerations, with 94 percent of those reviewed mentioning this as a high priority item. Ensuring as close to a pain-free experience as possible came next, with 81 percent of reports indicating this as an essential matter. In addition to patient opinions, even family members, who can understandably lean towards extending life and keeping loved ones close to medical professionals, were found to prioritize dying with dignity and maximizing their quality of life.
What can be done to improve hospice enrollment?
The solution to improving hospice enrollment starts with communication. Physicians need to do a better job of discussion treatment and prognosis with their patients and include hospice and palliative care as viable options. To date, there is no national or governmental training to help physicians with this matter, but many hospitals and hospices are working to improve the situation. In the immediate term, hospices can work with their referral networks to offer training and workshops to physicians, and to continue to promote education and awareness of end-of-life issues. Ultimately, patients will need to be given the final say on how to proceed with their final life transition, and physicians need to know how to ensure they carry out their patient’s wishes.